How Mouth Breathing and Airway Problems Can Cause Bedwetting
Why bedwetting is often a breathing and brain issue – not a behaviour problem.
By Dr Scott Wustenberg
D.C, FACNEM, M.Sc. NutMed (Distinction), B.Sc. Chiro, B.Sc. Physiology/Biochemistry
Bedwetting (nocturnal enuresis) is often seen as a “toilet training” problem, a deep sleep problem, or even a motivation problem.
But for many children – and even some adults – bedwetting is actually a sign of night-time breathing problems, such as:
- Airway blockage or narrowing
- Mouth breathing
- Snoring
- Airway blockage or narrowing
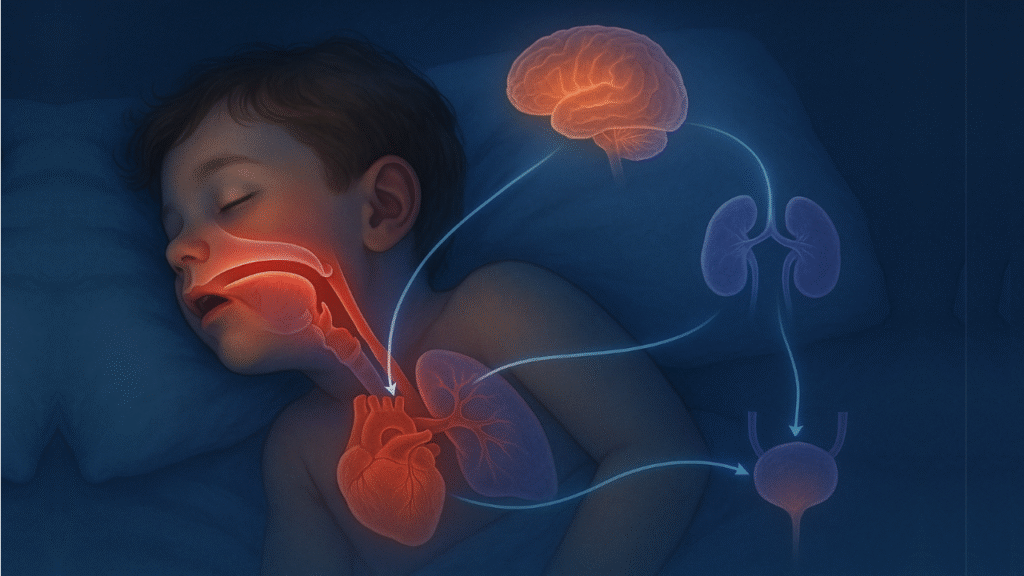
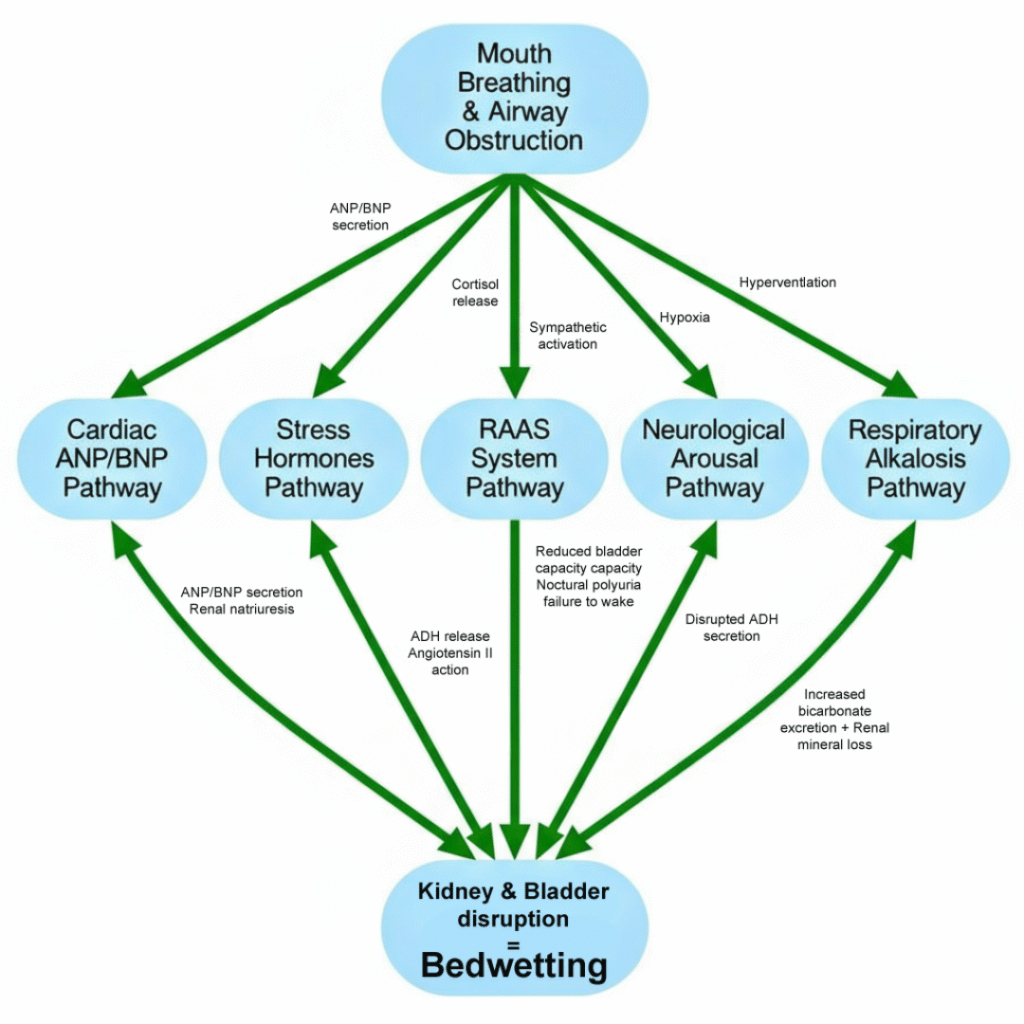
When the airway and breathing are not working well during sleep, it sets off a chain reaction in the body. Hormones change, blood pressure changes, kidney function changes, and even the bladder and brain’s waking system are affected. Together, these changes can easily lead to bedwetting.
This article explains the main pathways in simple language, so parents and health professionals can understand what is going on.
Breathing, the Heart, and the Kidneys: Why More Urine Is Made at Night
When a child’s airway is blocked or narrowed during sleep, they have to work very hard to breathe, activating many more neuromuscular systems especially in the chest. This creates strong negative pressure inside the chest.
This has two big effects:
1. The heart gets stretched
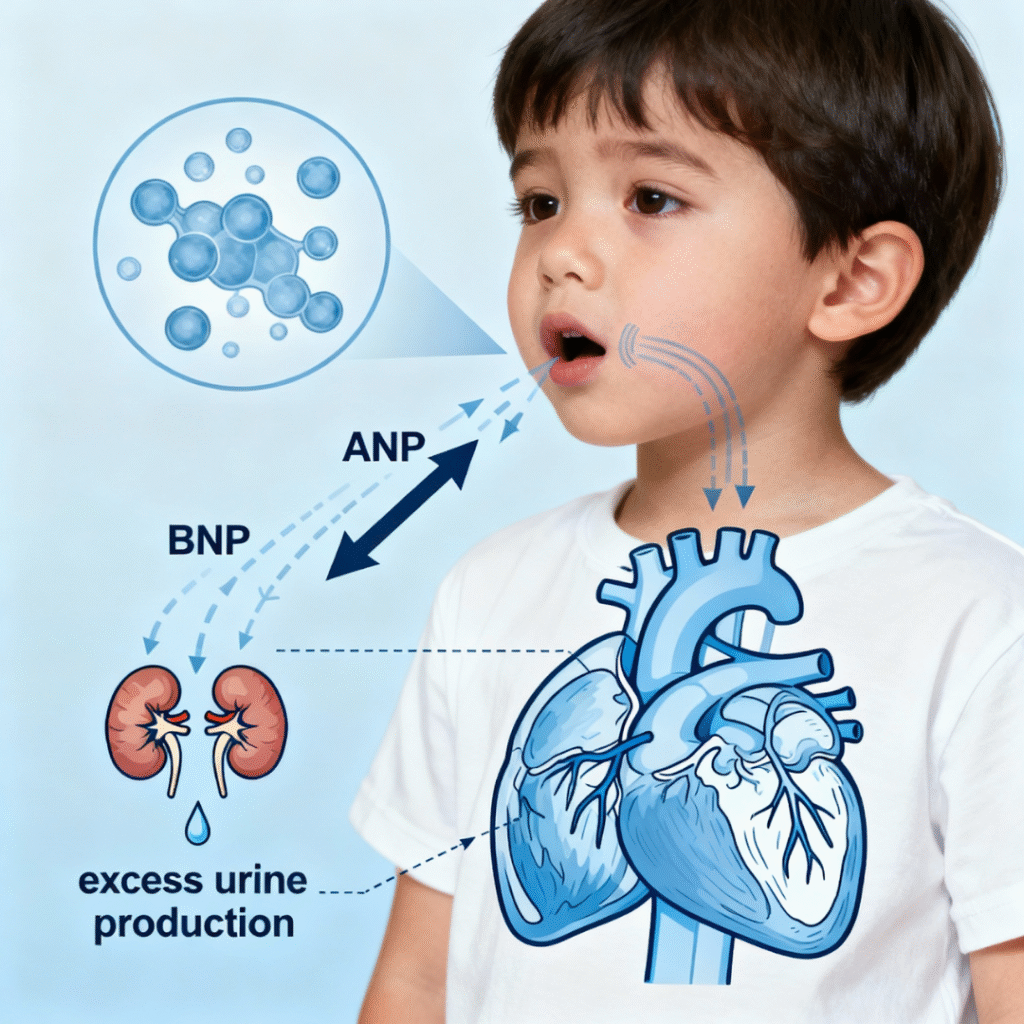
The extra pressure loads more blood into the heart due to increased venous return. The heart chambers stretch, and this stretch makes the heart release special hormones called ANP (atrial natriuretic peptide) and BNP (brain/ B-type natriuretic peptide).
2. These hormones tell the kidneys to get rid of extra fluid
ANP and BNP tell the kidneys:
- “Make more urine.”
- “Get rid of more salt and water.”
- “Turn down systems that normally help the body maintain fluid.”
The result is nocturnal polyuria – too much urine made at night.
The bladder fills faster than normal, and sometimes faster than the child can wake up.
Simple idea: Blocked breathing → heart stretch → heart hormones → kidneys turn on the “night-time tap”.
The Night-Time “Dry” Hormone Stops Working Properly (ADH)
Normally, the body is very smart at night. It releases more of a hormone called ADH (antidiuretic hormone). ADH helps you:
- Make less urine at night
- Make more concentrated urine
- Sleep through the night without needing to pee
But with sleep apnoea and airway problems:
- Sleep is broken by repeated mini-awakenings (even if the child doesn’t remember them).
- The normal night-time rise in ADH is disturbed.
- ANP and BNP from the heart also reduce ADH.
So instead of making less urine at night, the child makes more.
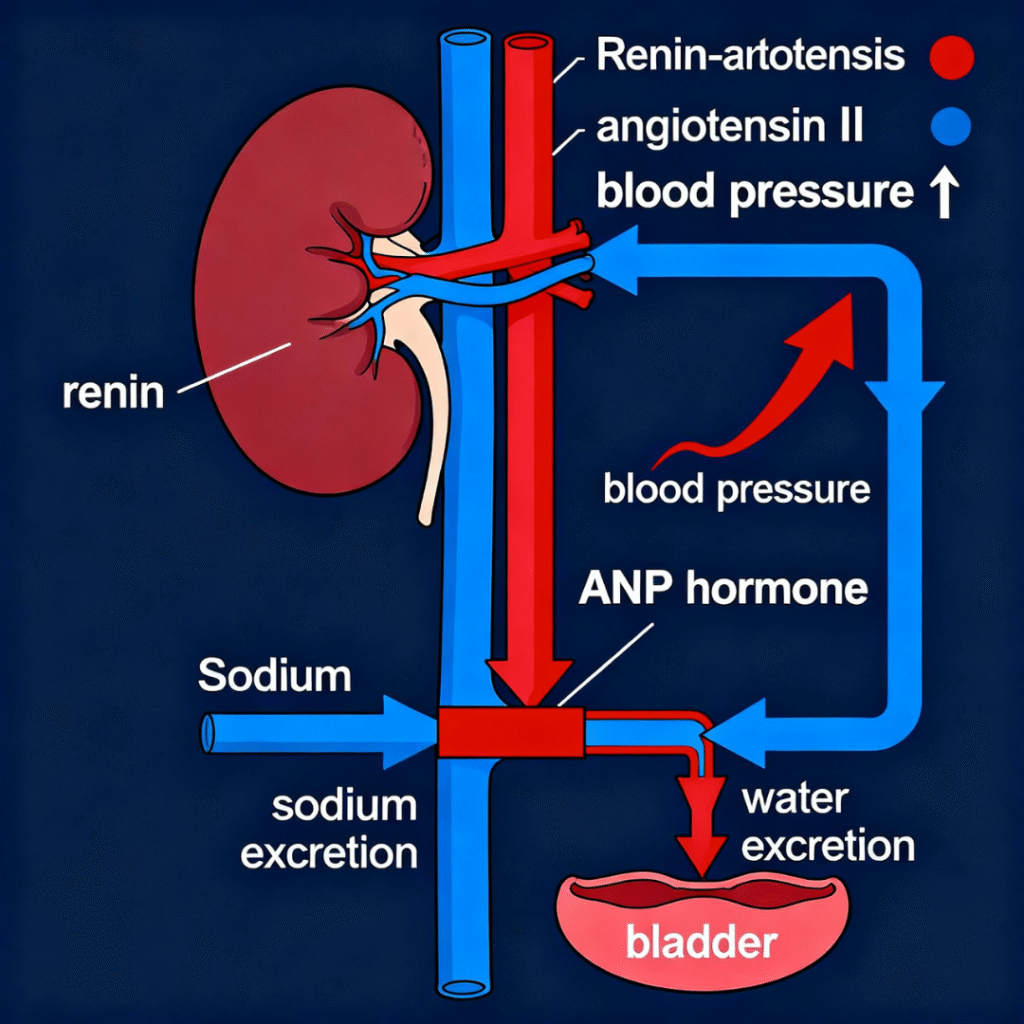
Stress Hormones: The Body Thinks the Child Is in Danger
Every time the airway closes, the body treats it like an emergency:
- Oxygen drops
- Carbon dioxide changes
- The child may briefly wake or almost wake
This activates the stress system:
- The HPA axis releases cortisol
- The sympathetic nervous system releases adrenaline and noradrenaline
This “bear in the room” response may help the child stiffen the airway or wake up enough to breathe again. But it has side effects:
- On the kidneys:
- Changes blood flow to the kidneys
- Alters how much salt and water are kept or released
- Affects how the bladder and its sensors behave
- On blood pressure:
- Blood vessels tighten
- Heart rate goes up
- Blood pressure spikes during and after apnoea events
- Over time, this can lead to higher daytime blood pressure
These stress hormones make the whole system more tense, including the bladder and the nerves that control it.

Deep but Broken Sleep: The Brain Can’t Wake to a Full Bladder
Many parents say, “My child sleeps so deeply; I just can’t wake them.”
Children with airway problems and bedwetting often have:
- More sleep fragmentation (lots of small interruptions to sleep)
- More deep sleep pressure (the brain “craves” deep sleep to make up for the poor quality)
- A higher arousal threshold – it is harder to wake them
This means that even when:
- The bladder is full
- The bladder sends “I need to go” signals
…the brain does not wake up in time.
Important: This is not laziness. It is a neurological and sleep problem created by breathing disturbance.
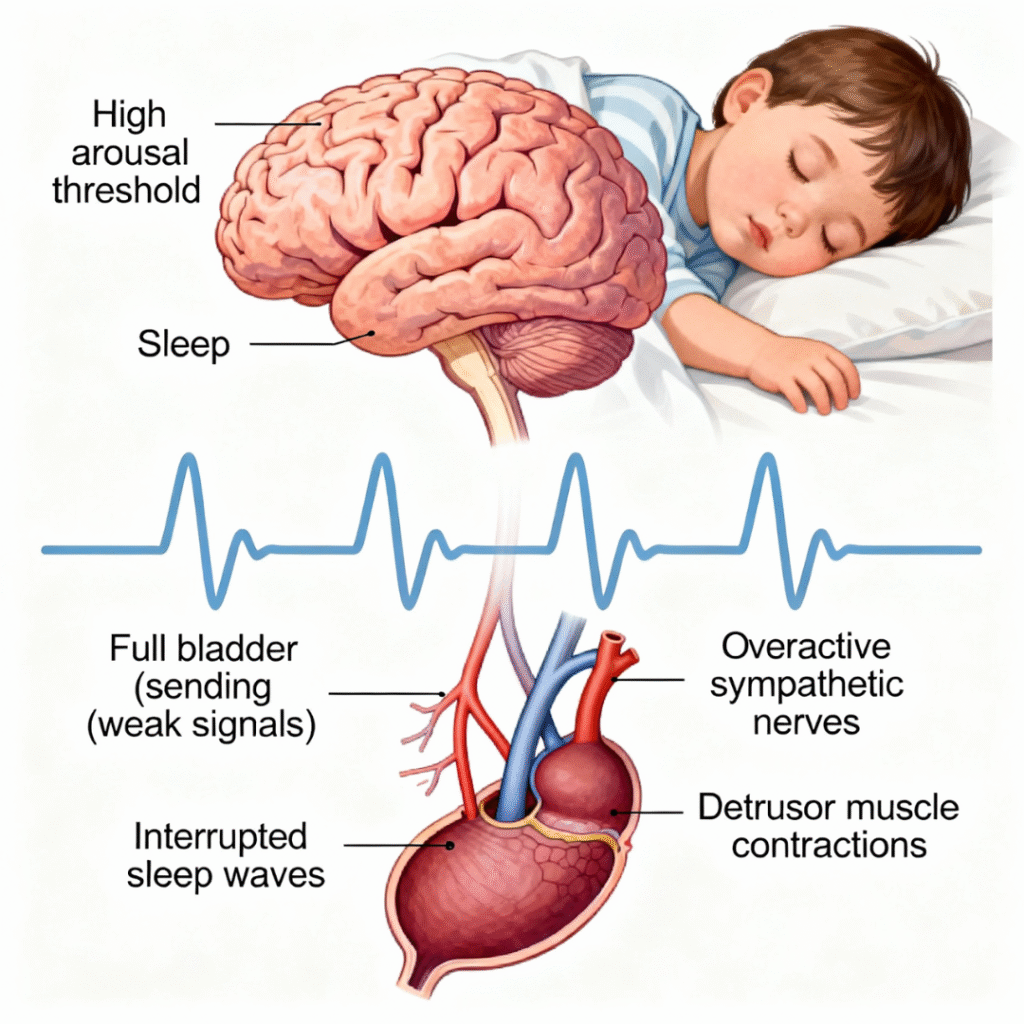
The Bladder Becomes Overactive and Irritable
Airway obstruction and low oxygen at night do not only affect the heart and kidneys. They can also affect the bladder itself.
Research shows that:
- Repeated low oxygen (intermittent hypoxia) can cause oxidative stress in bladder tissue.
- This can change the bladder muscle (detrusor), making it more likely to contract too early.
- The bladder wall may thicken over time, and its behaviour becomes unstable.
This is called detrusor overactivity:
- The bladder contracts before it is truly full.
- The effective bladder capacity is smaller.
Combine this overactive bladder with a child who cannot wake easily, and the outcome is predictable: bedwetting.
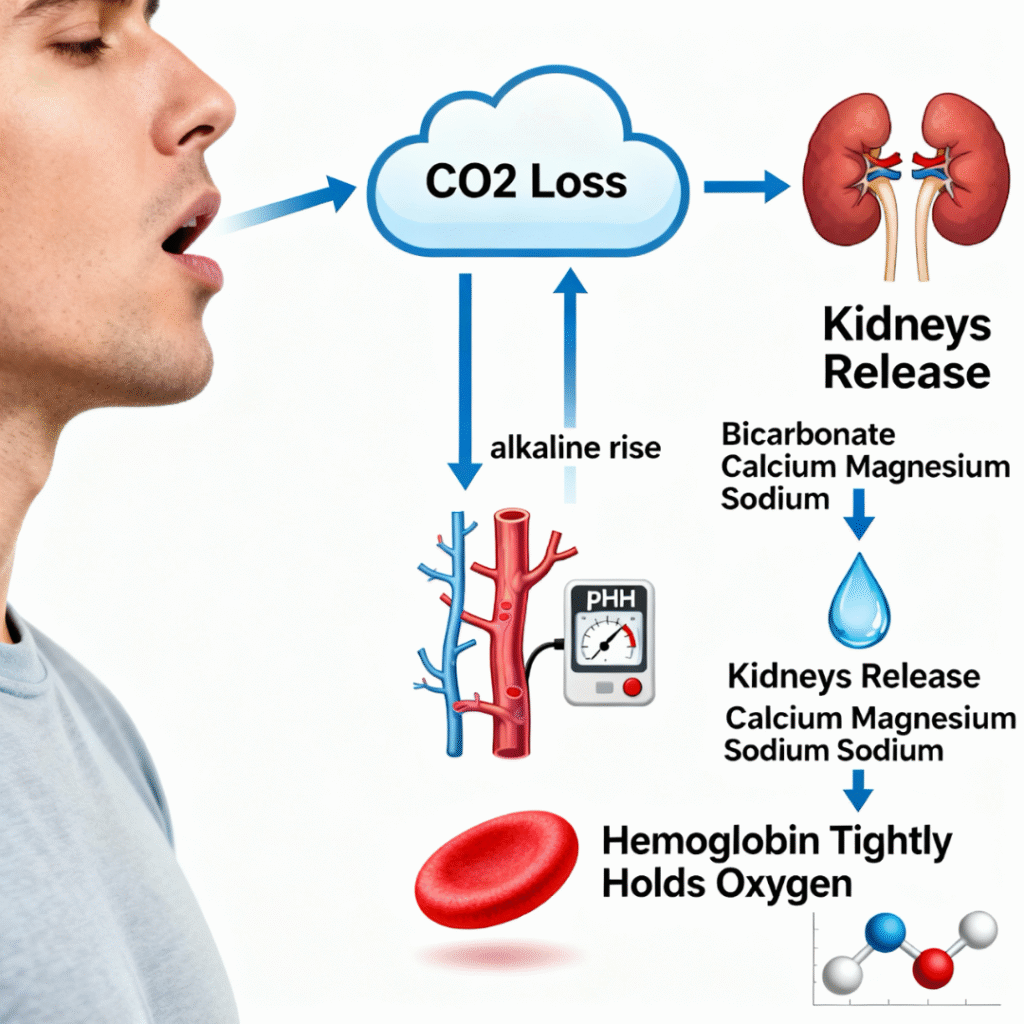
Mouth Breathing and Mineral Loss: The Metabolic Piece
Chronic mouth breathing can change how a child breathes out carbon dioxide (CO₂).
Often, mouth breathing is linked to over-breathing or mild hyperventilation:
- Too much CO₂ is blown off.
- Blood becomes more alkaline (called respiratory alkalosis).
The kidneys then try to fix this by:
- Getting rid of bicarbonate
- Also releasing important minerals like magnesium, sodium, phosphorus, and calcium into the urine
- Loss of some of minerals can cause a type 2 nutrient deficiency syndrome when it becomes chronic, effecting growth
These minerals are vital for:
- Muscle control (including the bladder muscle)
- Nerve function
- Energy production (ATP)
At the same time, a more alkaline blood pH makes it harder for red blood cells to release oxygen to the tissues. So, even if blood oxygen looks “normal”, the tissues can still be relatively starved of oxygen.
This adds another layer of:
- Poor tissue function
- Bladder and nervous system instability
- Night-time control problems
Putting the Puzzle Together
Let’s pull it all into one simple flow:
1. Airway obstruction and mouth breathing
→ Strong negative pressure in the chest
→ Heart stretch and stress on blood vessels
2. Heart hormones (ANP/BNP)
→ Kidneys make more urine and salt at night
3. ADH disruption
→ The normal “stay dry at night” hormone rhythm is disturbed
→ Less concentration of urine, more volume
4. Stress hormones (cortisol, adrenaline, noradrenaline)
→ Higher blood pressure
→ Changes in kidney function
→ Extra strain on the bladder
5. Direct effects on kidneys and bladder
→ Kidney tissue under stress from hypoxia
→ Bladder muscle becomes overactive and irritable
6. Sleep and arousal problems
→ Child sleeps deeply but poorly
→ Brain doesn’t wake when the bladder is full
7. Metabolic and mineral changes from mouth breathing
→ Loss of key minerals
→ Worse muscle and nerve control
End result:
- Too much urine at night
- An overactive bladder
- A brain that cannot wake in time
→ Bedwetting.
What Treatment Tells Us
When we treat the airway problem, bedwetting often improves or stops.
Studies show that in many children:
- Adenotonsillectomy (removing enlarged adenoids and tonsils) can reduce or even resolve bedwetting in a large percentage of cases.
- In adults, CPAP treatment for sleep apnoea often improves nocturia (night-time urination) and night-time accidents.
These treatments help by:
- Normalising pressure in the chest
- Reducing hypoxia (low oxygen) and stress hormone release
- Improving sleep quality and brain arousal patterns
- Reducing abnormal hormone signals to the kidneys
- Giving the bladder and kidneys a chance to recover
Emerging work with:
- Tethered oral tissue (TOT) release
- Airway-expansion orthodontics
also aims to improve airway size and function, and early reports suggest similar benefits, though more research is needed.
The key message is:
Bedwetting, when linked to sleep-disordered breathing, is not a behavioural issue. It is a medical and physiological problem that can often be improved by fixing the airway.
When Should Parents Seek Help?
Parents may want to talk to a health professional experienced in airway and sleep if:
- The child snores regularly, (even if only very quietly)
- The child mouth breathes during the day or night
- There are pauses in breathing or gasping during sleep
- The child is hard to wake in the morning, tired, or has behaviour/attention problems
- Bedwetting continues beyond the usual age or returns after being dry
A team approach can help, including:
- Medical doctors (e.g. paediatrician, ENT)
- Dentists / orthodontists with airway and TOT focus
- Oral Myofunctional therapists
- Sleep and breathing specialists
For Clinicians and Curious Readers
This article is a simplified overview of a much more detailed biochemical and physiological model.
For those who would like to see:
- The full technical explanation of each pathway
- Detailed discussion of cortisol, catecholamines, RAAS, renal hypoxia, detrusor changes, and respiratory alkalosis
- A complete reference list

