NASAL BREATHING VS MOUTH BREATHING

Great Breathing is Nasal Breathing
Humans are meant to breathe through the nose and not the mouth, except when running, or if you have a cold. There is a functional strong innate preference for nasal breathing with the airways performing several important jobs including:
- Filtering air with cilia/hair
- Filtering with nasal mucosa
- Humidifying
- Heating
- Adenoids and then tonsils cleaning the air inflow
If the mouth is open to breath all the cleaning is done by the tonsils in the pharynx. This is not ideal and is especially worse by environmental loads such as mould spores, dust, bacteria etc. It can lead to infections, tonsilitis, and lung issues.
- Regular mouth breathing leads to greater difficulty in nasal breathing as the sinuses can fill and thicken with mucous, making it harder to breathe through the nose and a condition called upper airway resistance syndrome (UARS)especially during sleep.
- Enlargement of the tonsils can occlude the airway both from nasal and mouth breathing and contributes to snoring and apnoea.
The mouth structure is super important for breathing function and great sleep.

- In a normally developing child, the lips and cheek muscles act as one part of the jelly mould to shape the optimal mouth and airway structure.
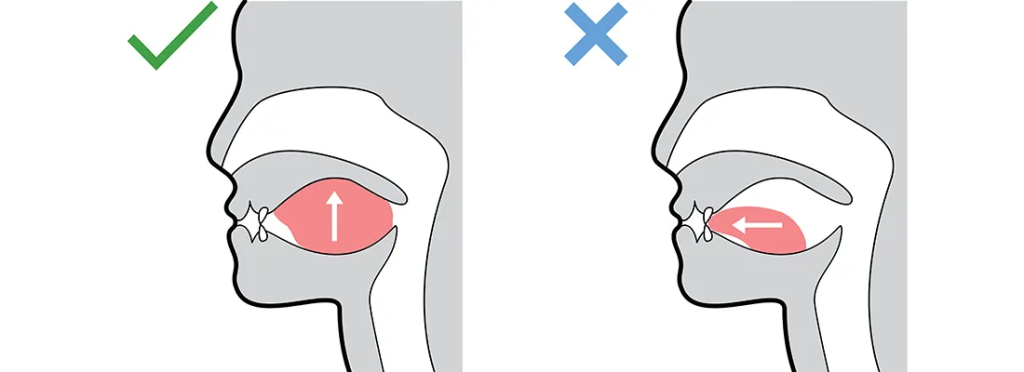
- The unrestricted tongue thrusts up and forward into the roof of the mouth with sucking, eating (and later on talking) which drives optimal maxilla and jaw development.
- Optimal structure is a dome shaped arch, like the cysteine chapel, if the tongue sits down in the mouth the bone development is not adequately splayed and results in suboptimal bone development and short rami (short face in an A-P direction) causing teeth to become crowded in the
jaws. - Poor development, and mouth breathing creates a maxilla that has a gothic chapel roof, narrow and tall, which impacts on the nasal air space, leads to septal deviation, especially after orthodontic involvement.
The four elements of good posture of the tongue and mouth

- Tongue lightly suctioned to the roof of the mouth when not in use.
- Lips gently sealed without strain or muscle activation.
- Nasal breathing
- No activity of the muscles around the mouth during subconscious swallowing
This scenario is encouraged by discouraging habits such as use of pacifiers/dummies, or finger/thumb sucking, along with prolonged snippy cup use. These habits all alter lip seal and alter activation in the muscles of the mouth, leaving the lips apart and greater capacity for bacteria to enter the oral cavity with susceptibility to infection of teeth, dental cavities and tonsil and sinus issues.
Myofunctional Disorders of the Mouth and Face
Any time the muscles of the face or mouth do not work correctly this is labelled a myofunctional disorder. Regardless of age of patient. This includes:
- During suction
- Swallowing
- Breathing
- Chewing
- Speech
However, from a developmental point of view, form follows function. Thus, before you see the crooked crowded teeth or high arch or large tonsils, we can see the warnings signs which herald later issues.

From the book Sleep Breath thrive, myofunctional disorders include:
- Open mouth breathing
- Infant latching or sucking problems
- Poor swallowing and excessive air intake while feeding
- Reflux like symptoms in infancy
- Tongue/lip/buccal ties
- Use of pacifiers/finger/thumb sucking
- Overuse of pouch foods bottles and or snippy cups.
- Nasal obstruction enlarged tonsils and adenoids
- Allergies and nasal congestion
- Poor swallowing and estuation tube clearance – recurrent ear infection or glue ear
- Soft overly processed diets which require little chewing
- Chewing and swallowing difficulties
- Messy open mouth chewing
- Drooling
- Snoring
- Teeth grinding clenching brutish
- Lisps, speech articulations issues, particularly with n, l, a, d, s and z
- Nail biting
- Chewing on clothes hair or objects
- Other consequences of oral myofunctional disorder can be seen with picky eating or a preference for soft food
- The tongue thrusting between the teeth to help Form
- Choking during mealtimes
- The need for liquid during meals to help the swallow
- Excess and inappropriate placement of tension on the lips.
Consequences of Nasal Breathing:
Nasal breathing is a pillar of health generally and without it, disease progression is a slow grind onwards.

The obvious signs of which will be seen with:
- Dry mouth in the patient,
- Chapped lips from the air going across them all the time,
- Bad breath
- Inflamed gums
- Gingivitis
- Increase dental decay and plaque due acidification of the mouth
- Decline in the saliva production
Other signs not directly expected but related:
- Increased tension in the neck, scalp, and facial muscles especially around the jaw.
- Sufferers are more likely to have migraines and tension headaches, this can be due to low oxygen as well as from acidification, and over activation of muscle spindles.
- Trigger points and pain syndromes.
Think about this from a recruitment point of view, if you’re having difficulty breathing due to airway occlusion the brain recruits more muscles and increases tension in them until airflow is achieved or until you wake up, this also can occur during wake times, especially due to poorly learned breathing habits.
The neck-derived headaches are termed cervicogenic headaches and are common in URSA sufferers. These patients will commonly attend the chiropractor, physio, osteopath, or massage therapist on a regular basis to seek relief from the “My neck and shoulders are always tight” complaint.
Sadly, the therapy does not last long, and the tension rebuilds, due to the issue occurring as a defence mechanism to protect airway while asleep.

- Increased risk of upper airway problems including rhinitis, sinusitis, and ear infections.
- This commonly is linked to increased use of antibiotics along with enlarged tonsils and adenoids
- It is an independent factor in the etiology of asthma.
Tongue Mouth and Breathing Effect Sleep, Apnoea and Hypopnea (OAFMS)
The tongue posture is an essential element of craniofacial development and is integrated into CNS (central nervous System) development.
Tongue posture is altered by mouth breathing , while poor tongue posture can also lead to mouth breathing especially during REM phases of sleep when the muscle paralysis occurs, and tone lowers in the sleep cycle.
Poor Tongue tone and posture contributes to apnoea and hypopnea events, leading to lower blood oxygen saturation and increased carbon dioxide in the blood stream.
The increase in CO2 creatures a shift in the acid base balance of the blood leading to acidification. Acidification in the blood stream, causes increase calcium release and muscle tension.
This could also place stress on the pancreas where bicarbonate is made and released to keep pH in range. Alteration in calcium metabolism may have implications for bone development and calcification of the facial and jaw structure in a developing child.
Open mouth breathing for any reason is associated with a phenomenon called cranial developmental drift, both causally in infants and children, and as a result of cranial maldevelopment.
As the children’s face slowly deviate away from normal growth pattern, this leads to an adult with structural postural change including a long face, narrow through the jaw and maxilla, this is also called an adenoid face.
Maldevelopment patterns include:
- More prominent protruding teeth
- Incapacity to keep the lips sealed
- Retrusion of the mandible
- Slackening off the jaw and jaw muscles
- Teeth will then tend to become crowded and crooked
The narrow palette with the high arch is an airway risk factor which is associated with disturbed sleep and breathing (OSA) leading to consequences in adulthood.
Consequences of Mouth Breathing:

Mouth breathing is associated with an increase in airway resistance termed upper airway resistance syndrome (UARS) by 2.5 times. The consequence is:
- Airway collapsibility
- Snoring
- OSA
- Hypopnea
- Reduced restive sleep
This is not surprising as the airway must be defended by the brain at all costs to maintain oxygen supply.
The brain will release catecholamines (cortisol and adrenaline) to tighten the airway, and partially raise the body out of the sleep state to a greater level of consciousness and alertness without full consciousness of this occurrence. This is termed sleep fragmentation.
Fragmentation of sleep is associated with many long-term consequences:
- Increased il6 production
- Increased blood sugar
- Insulin resistance
- Weight gain
- Hormonal dysregulation
- Social emotional problems
- Depression
- Anxiety
- Chronic high amounts of iL6 release is shown to damage the serotonergic receptors and increase pain sensitization
The emotional dysregulation makes a lot of sense given that the brain is a pattern and sense generator trying to make sense of the world.
If it senses the bloodstream/body is filled with stress/threat hormones then it runs the threat program, sadly if you cannot find the cause of the threat, as the monster is not in the room (it’s your tongue/airway choking you in your sleep when you did not see it with your conscious brain) it will leave you uneasy and constantly looking for the monster, this resembles vigilance and anxiety.
Signs of Sleep Apnoea in Children:

- Snoring: Children with sleep apnoea may snore loudly and frequently during sleep.
- Breathing pauses: Children with sleep apnoea may have periods of time during sleep where they stop breathing or have shallow breathing.
- Restless sleep: Children with sleep apnoea may have trouble sleeping through the night and may be restless or thrash around in bed.
- Daytime sleepiness: Children with sleep apnoea may be excessively tired or have difficulty staying awake during the day.
- Bedwetting: Children with sleep apnoea may experience bedwetting due to the disrupted sleep caused by the condition.

