APNEA, HYPOPNEA AND SLEEP FRAGMENTATION
Understanding Sleep Apnea, Hypopnea, and Sleep Fragmentation in Adults
Sleep apnea, is a prevalent sleep disorder affecting millions globally, disrupts breathing during sleep, leading to poor-quality rest and various health issues. This article delves into the effects of sleep fragmentation and obstructive sleep apnea (OSA) in adults, offering comprehensive insights for better understanding.
Factors Contributing to Adult Onset of Sleep Apnea


Tongue Tie and Airway Restriction
The emergence of adult-onset sleep apnea can be attributed to several key factors, each playing a distinct role in creating conditions conducive to the disorder. One significant contributor is the presence of tongue tie, a condition wherein the movement of the tongue is constrained. This limitation can lead to airway restriction during sleep, heightening the likelihood of interrupted breathing episodes.
Cranial Maldevelopment and Orthodontic History
Cranial maldevelopment, whether occurring independently or linked to a history of orthodontic treatments, emerges as another influential factor. Irregularities in cranial development can compromise the structural integrity of the airway passages, establishing an environment conducive to the development of sleep apnea.
Obesity-Related Weight Gain
The well-established risk factor of obesity further compounds the scenario. Excessive weight gain, particularly around the neck and throat region, exerts added pressure on the airway. This heightened stress increases the susceptibility to airway collapse during sleep, contributing to the occurrence of apneas and hypopneas.
The interplay of factors such as tongue tie, cranial maldevelopment, and obesity-related weight gain creates a multifaceted scenario that predisposes adults to the onset of sleep apnea. Understanding these contributing elements is crucial in comprehending the origins of the disorder and formulating effective strategies for both prevention and management.

Understanding Sleep Apnea
Sleep apnea is a sleep disorder characterized by the recurrence of obstructive apnea and hypopneas, poses unique respiratory challenges during sleep. Taking a closer look at its definition sheds light on the complexities of this condition.
Obstructive Sleep Apnea (OSA)
The primary manifestation of sleep apnea is Obstructive Sleep Apnea (OSA), frequently abbreviated as OSA. In OSA, a pause in respiration lasting over 10 seconds occurs at least five times per hour. This interruption is primarily attributed to a blockage in the airway, where the flow of air is impeded, resulting in a temporary cessation of breathing. Various factors, including the relaxation of muscles and tissues during sleep, contribute to the characteristic pauses in breathing.
Central Sleep Apnea (CSA)
On the other hand, Central Sleep Apnea (CSA) represents a distinct type of sleep apnea characterized by a lack of respiratory effort. Unlike OSA, where physical obstruction is the primary issue, CSA involves a failure of the central respiratory control system. This leads to a temporary cessation of breathing without concurrent efforts to resume airflow. The crucial distinction lies in the absence of respiratory muscle activity during these episodes, providing a diagnostic difference from the obstructive variant.
Exploring Hypopnea
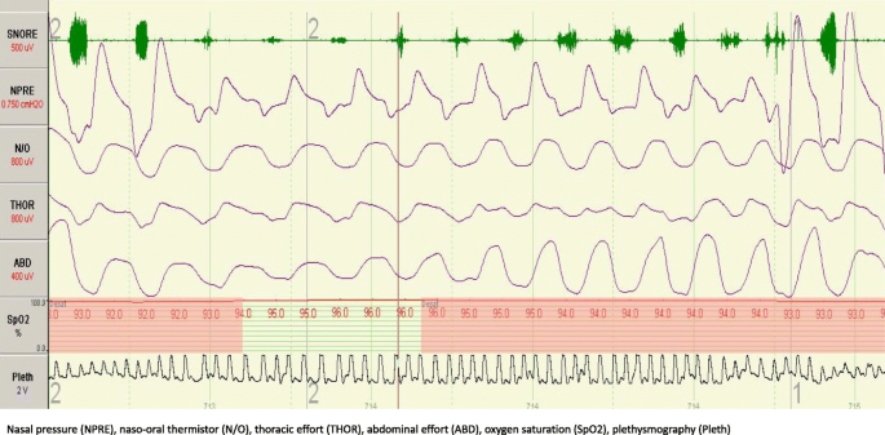
Photo credits to sleep.biomedcentral.com
Let’s delve into the realm of hypopnea, a distinctive facet of sleep-disordered breathing that brings about significant alterations during sleep and warrants a closer examination of its intricacies and potential impact on overall health.
Ventilation Reduction
At its core, hypopnea is characterized by a noteworthy reduction in ventilation, with a marked decrease of 50% or more in airflow. This reduction poses a substantial challenge to maintaining optimal respiratory function during sleep
Arterial Saturation Decline
One consequential outcome of hypopnea is the subsequent decline in arterial saturation. This decline is quantified by a reduction of 4% or more in the oxygen levels carried by the blood. Such shifts in arterial saturation levels can have profound implications for overall health and well-being, particularly when recurring throughout the sleep cycle.
Partial Airway Obstruction
The genesis of hypopnea lies in partial airway obstruction during sleep. Unlike the complete blockage observed in apnea, hypopnea involves a partial hindrance to airflow. This obstruction is often associated with relaxed or collapsed airway structures, contributing to the reduction in ventilation.
Associations with Daytime Sleepiness and Cardiopulmonary Function
Notably, hypopnea frequently correlates with daytime sleepiness, stemming from disrupted sleep patterns and compromised sleep quality. Additionally, challenges posed by hypopnea may manifest in alterations to cardiopulmonary function, impacting the optimal functioning of the heart and lungs.
Understanding these facets of hypopnea provides insights into its nuanced nature and the potential repercussions it may have on both sleep and overall health.
Causes of Apnea and Hypopnea

Let’s explore the origins of apnea and hypopnea, rooted in the intricate dynamics of the respiratory system during the vulnerable state of sleep. Understanding the causes of these disruptions provides insight into the physiological changes that contribute to the interruption of normal breathing patterns.
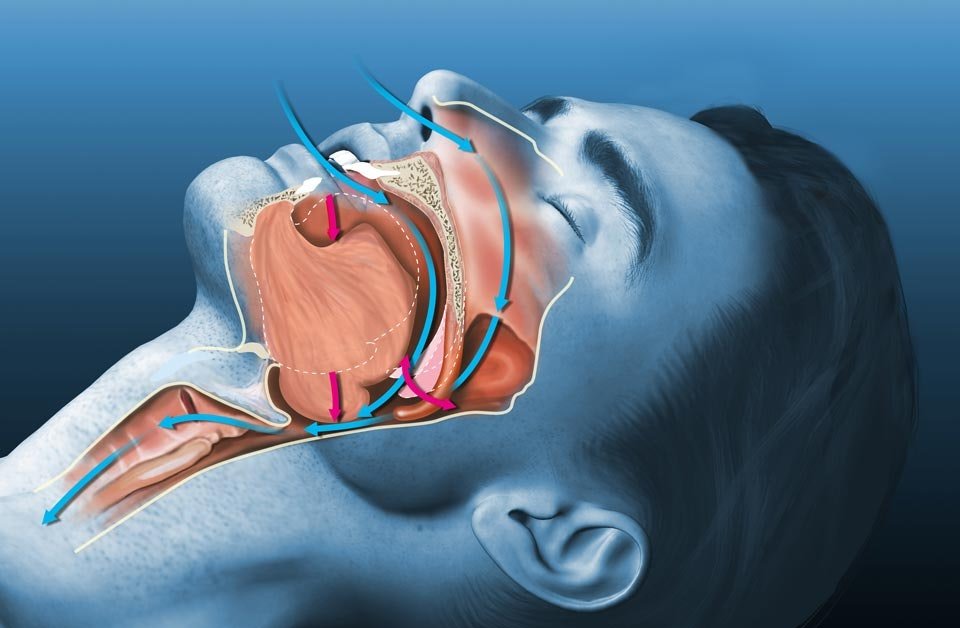
Airway Closure during Inspiration
Apnea and hypopnea are fundamentally rooted in the closure of the airway during the inspiratory phase of breathing while asleep. This closure, occurring during attempts to inhale, becomes a pivotal event leading to interruptions in the regular respiratory rhythm.
Muscular Relaxation during Sleep
The act of sleep induces a comprehensive relaxation of all muscles, including those in the airway, neck, and throat. While this natural relaxation is essential for restorative sleep, it presents challenges when it compromises the patency of the airway.
Dysregulation in OSA
In the case of Obstructive Sleep Apnea (OSA), individuals face a specific challenge where the dilating muscles responsible for maintaining airway openness struggle to counteract negative pressure during inspiration. This struggle compromises the ability to keep the airway unobstructed, leading to instances of partial or complete blockages.
Impact of Negative Pressure
A critical factor in the genesis of apnea and hypopnea is the impact of negative pressure within the airway during inspiration. In the context of OSA, the normal physiological response to negative pressure, typically maintained by dilating muscles during wakefulness, weakens during sleep. This weakening allows negative pressure to exert undue influence, potentially causing the airway to collapse or become significantly narrowed. Understanding these mechanisms sheds light on the complexities underlying disrupted breathing patterns during sleep.
The Impact of Tongue Tie on Sleep-Related Airway Obstruction

Let’s explore how the presence of tongue tie can significantly impact the dynamics of the airway during sleep, potentially aggravating issues related to breathing interruptions. Understanding the role of tongue tie is crucial for gaining insights into how this anatomical condition contributes to disrupted breathing patterns during sleep.
Restricted Tongue Movement
Tongue tie, scientifically known as ankyloglossia, refers to a condition where the movement of the tongue is restricted due to an abnormally short, thick, or tight band of tissue beneath the tongue. This restriction can hinder the natural range of motion of the tongue, affecting its ability to perform essential functions, including the maintenance of optimal airway patency.
Contribution to Airway Narrowing or Blockage
In individuals with tongue tie, the limited movement of the tongue may play a pivotal role in further narrowing or blocking the airway during sleep. As muscles naturally relax during the sleep cycle, the constrained mobility of the tongue can contribute to an increased likelihood of airway obstruction.
Episodes of Interrupted Breathing
The significance of the compromised airway, stemming from restricted tongue movement, becomes particularly pronounced during sleep. This limited mobility, coupled with the natural relaxation of muscles, may result in episodes of interrupted breathing. Such episodes can manifest as apneas or hypopneas, contributing to sleep fragmentation and a decrease in the overall quality of rest. Understanding these mechanisms sheds light on the specific ways in which tongue tie can impact sleep-related airway obstruction.
Manifestations and Distinctive Characteristics of Sleep Apnea

Let’s delve into the varied manifestations and distinctive characteristics of sleep apnea, a condition marked by a spectrum of features that collectively contribute to its complexity and potential impact on various physiological parameters. Gaining an understanding of these unique traits provides a comprehensive overview of the multifaceted nature of sleep apnea.
Hypoxemia
Sleep apnea frequently gives rise to hypoxemia, a condition characterized by lower-than-normal levels of oxygen in the blood. The recurring interruptions in breathing result in diminished oxygen saturation, affecting the overall delivery of oxygen to vital organs and tissues.
Hypercapnia
Simultaneously, sleep apnea may contribute to hypercapnia, an elevation in carbon dioxide levels in the blood. The inadequate exchange of oxygen and carbon dioxide during interrupted breathing episodes can disrupt balance, leading to increased carbon dioxide retention.
Large Intrathoracic Pressure Swings
A noteworthy consequence of sleep apnea events is the substantial fluctuation in intrathoracic pressure, the pressure within the chest cavity. These significant pressure swings result from the struggle to breathe against airway resistance, thereby adding stress to the respiratory system.
Surges of Systemic Blood Pressure
Sleep apnea episodes are often accompanied by surges in systemic blood pressure. Intermittent periods of reduced oxygen supply trigger compensatory mechanisms, leading to elevated blood pressure levels. Over time, these surges can contribute to cardiovascular strain and complications.
Associated Arousals and Sleep Fragmentation
Sleep apnea disrupts normal sleep architecture, causing frequent arousals and sleep fragmentation. The body’s response to breathing interruptions prompts partial awakenings, preventing individuals from reaching deeper, more restorative sleep stages.
Severe Sleep Fragmentation Frequency
In severe cases of sleep apnea, sleep fragmentation may occur at an alarming frequency, reaching up to 100 times per hour. This heightened level of sleep disruption underscores the severity of the condition, exacerbating the impact on overall sleep quality and contributing to daytime sleepiness and impaired cognitive function. Understanding these nuanced characteristics provides valuable insights into the diverse repercussions of sleep apnea on both sleep and physiological well-being.
Implications for Disease Progression

Exploring the distinctive characteristics associated with sleep apnea reveals a pivotal role in shaping the trajectory of disease progression, impacting various aspects of an individual’s health. Understanding these implications provides insights into the broader consequences and helps elucidate the potential challenges that individuals with sleep apnea may face.
Cardiovascular Consequences
The cardiovascular consequences of sleep apnea, including hypoxemia, hypercapnia, and blood pressure surges, contribute significantly to increased cardiovascular strain. Over time, this can lead to the development or worsening of cardiovascular conditions, such as hypertension, heart disease, and an elevated risk of stroke.
Neurocognitive Effects
Sleep fragmentation and associated arousals disrupt the natural sleep cycle, resulting in neurocognitive effects. Individuals with sleep apnea may experience impaired memory, concentration, and cognitive function. Prolonged sleep disruption can contribute to the development of neurocognitive disorders over time.
Metabolic Impact
The physiological stress imposed by sleep apnea has implications for metabolic processes. Changes in oxygen and carbon dioxide levels, along with disruptions in sleep patterns, may influence metabolic dysfunction, insulin resistance, and an increased risk of type 2 diabetes.
Daytime Functioning
Sleep apnea’s repercussions extend to daytime functioning, with individuals often grappling with excessive daytime sleepiness, fatigue, and a decreased ability to perform daily tasks. These consequences can impair quality of life, work productivity, and overall well-being.
Quality of Life and Emotional Well-being
The cumulative impact of sleep apnea on physical health, coupled with the emotional toll of disrupted sleep, significantly affects an individual’s quality of life. Mood disturbances, increased stress, and a heightened risk of mental health disorders may accompany the persistent challenges posed by sleep apnea. Understanding these intricacies provides a comprehensive picture of the multifaceted impact of sleep apnea on both physical and emotional well-being.
Conclusion
This exploration into sleep apnea, hypopnea, and sleep fragmentation underscores the significance of understanding these sleep disorders. Recognizing their origins, characteristics, and potential consequences provides a foundation for proactive health management. From the intricate dynamics of respiratory challenges to the impact on overall well-being, this journey through sleep health unveils crucial insights. Armed with this awareness, individuals are empowered to prioritize their sleep and seek tailored interventions, fostering a path to improved vitality and a more fulfilling life. Embracing sleep awareness emerges not only as a key to restful nights but as a fundamental pillar for holistic well-being.

Frequently Asked Questions
What is the main cause of sleep apnea?
The main cause of sleep apnea is often the relaxation of throat muscles and tissues, leading to airway obstruction during sleep.
How do you fix sleep apnea?
Sleep apnea can be addressed through lifestyle changes like weight loss and positional therapy. Using a Continuous Positive Airway Pressure (CPAP) machine is a common solution, and in certain cases, surgical interventions may be considered.
What are the warning signs of sleep apnea?
The warning signs of sleep apnea include loud snoring, abrupt awakenings with a choking or gasping sound, excessive daytime sleepiness, difficulty staying asleep, and morning headaches.
Can sleep apnea go away?
Sleep apnea may not completely disappear, even with lifestyle changes and treatments. Ongoing management is typically needed for effective symptom control.
Can you live a long life with sleep apnea?
Yes, it is possible to live a long life with sleep apnea through proper management and treatment. Seeking medical advice and adhering to recommended treatments are crucial for a positive outcome.
Is sleep apnea easy to fix?
Fixing sleep apnea often requires lifestyle adjustments and, in some cases, the use of medical devices like CPAP machines. While ongoing management may be necessary, there are effective solutions available.
What are 4 symptoms of sleep apnea?
The 4 common symptoms of sleep apnea include loud snoring, frequent pauses in breathing during sleep, abrupt awakenings with choking or gasping, and daytime sleepiness or fatigue.
Can stress cause sleep apnea?
Yes, stress can contribute to sleep apnea or exacerbate existing symptoms. Managing stress through relaxation techniques may help improve sleep quality for some individuals.
Which sleeping position is best for sleep apnea?
The best sleeping position for sleep apnea is sleeping on your side. It is often recommended for individuals with sleep apnea, as it can help keep the airway open and reduce the likelihood of breathing interruptions during sleep.


I’m trulyy enjoying the design and layout of your
site. It’s a very easy on the eyes which makes it much more enjoyable
ffor mme to come here and visit more often. Did you hire out a designer to create yyour
theme? Exceptional work!